As you probably already know, antibiotics are extremely important in modern medicine. Throughout history, millions of people have died from bacterial infection, and many millions more have been saved because of the discovery of antibiotics. Antibiotics are not effective against viral infections and can work by killing microbes or preventing/inhibiting their growth. Some, such a penicillins and cephalosporins, operate by damaging/compromising the cell wall and/or membrane of a particular bacterial cell. They are also able to inhibit particular enzymes that are necessary for the function of a bacterial cell. Other types affect a bacterial cell's ability to synthesize proteins and are referred to as bacteriostatic.
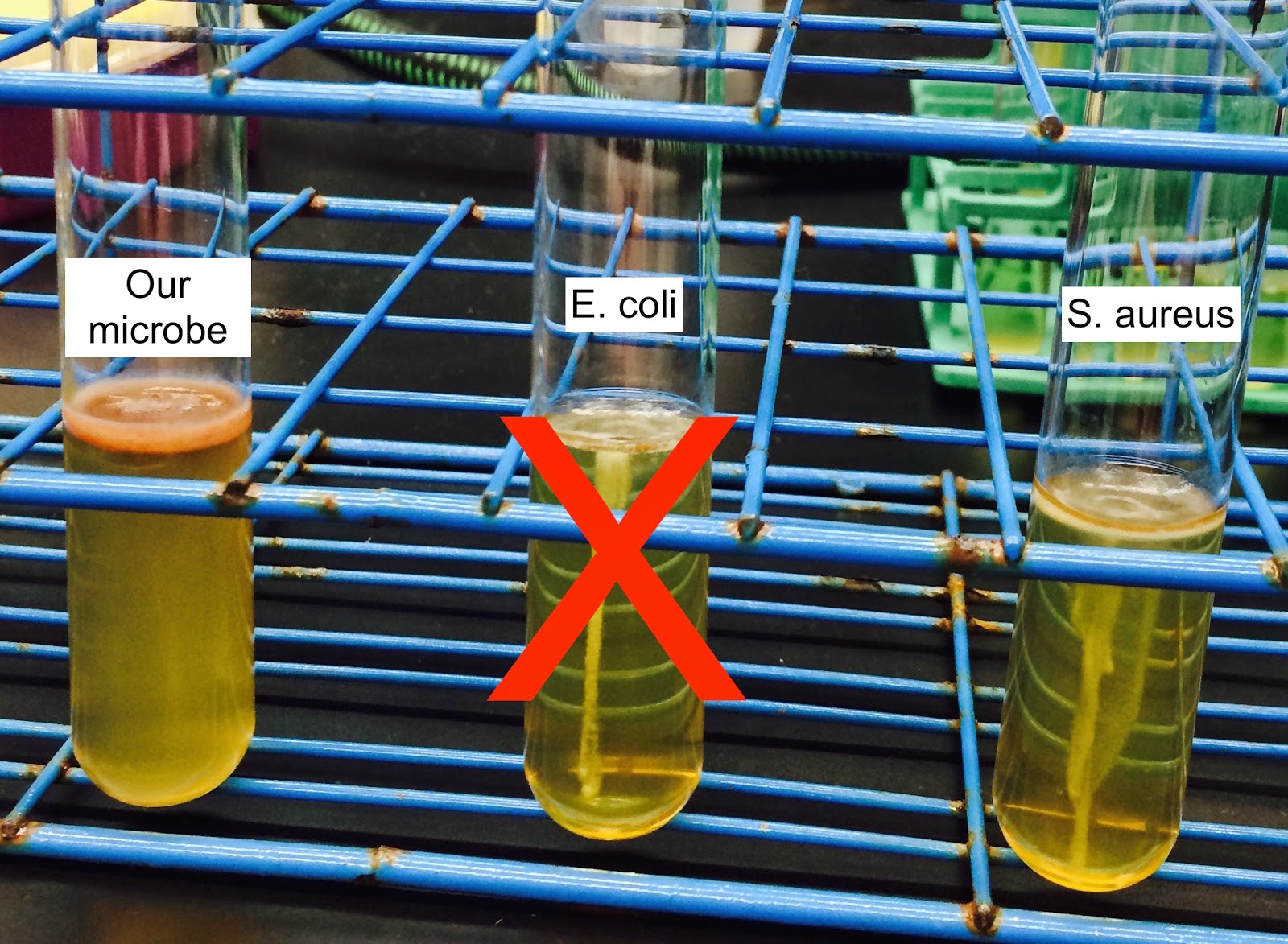
In this week's lab, several bacterial controls and our unknown microbe were plated so that a they grew "lawns." Before incubation, several antibiotic disks of varying types and concentrations were placed on each plate (see photos below). Later, they were each observed to determine whether they were sensitive (unable to grow in the presence of the antibiotic) or resistant (able to grow in the presence of the antibiotic).
 | |
|
 | |||
|
 | |
|
Antibiotic
Sensitivity
Microbes Tested
|
Tetracycline [30]
|
Ampicillin [10]
|
Carbenicillin [100]
|
Azithromycin [15]
|
K. pneumonia
|
Sensitive
|
Resistant
|
Sensitive
|
Sensitive
|
S. aureus
|
Sensitive
|
Sensitive
|
Sensitive
|
Sensitive
|
E. coli
|
Sensitive
|
Sensitive
|
Sensitive
|
Sensitive
|
Unknown
|
Sensitive
|
Resistant
|
Resistant
|
Sensitive
|
So what is the classification of our unknown microbes? Well using the results from previous weeks, we still believe that our unknown microbe is either clostridium, mycobacterium, or nocardia.
With further research into the possible identifications of our microbe, we discovered that the three possible classifications are categorized as producing beta lactamase. These enzymes break down the antibiotics making the microbes resistant, especially to penicillin-like antibiotics. This information is also supported by the antibiotics that our microbe is sensitive to because these antibiotics are not beta-lactamases.
To further verify our microbe, we would consider reconducting the acid-fast stain to confirm that we did the procedure properly and support our initial prediction of our microbe being mycobacterium or nocardia. An additional test to determine if our sample is clostridium would be to perform a starch hydrolysis test. This would allow us to determine if our sample is amylase-positive or negative. If amylase-positive, this would support our microbe's identification as clostridium.
After learning so much about our soil microbe, we recommend that you beware of the unique but dirty little creatures hiding all over our campus.
Thanks for tuning in all semester long!
Austin and Anne
http://en.wikipedia.org/wiki/Antibiotics
Mechanisms of beta-lactam resistance in anaerobic bacteria.
Beta-Lactamase Production and Resistance to Beta-Lactam Antibiotics in Nocardia
Genetic analysis of the beta-lactamases of Mycobacterium tuberculosis and Mycobacterium smegmatis and susceptibility to beta-lactam antibiotics.
http://www.austincc.edu/microbugz/starch_hydrolysis.php
http://www.uwyo.edu/molb2210_lab/info/biochemical_tests.htm#spirit_blue